Recently I responded to a blog that was decrying the lack of male contraception. I wish I had better news on that front, but there is good news about women’s birth control.
In response to the question: “Why do women have to take the hit of contraception?” I wrote that I am a retired male OB-GYN who has had a vasectomy. I believe in contraception for men! The blog”s author only listed two male methods: condom and vasectomy. She apparently didn’t know about withdrawal.
In the 1980s I practiced in Puerto Rico where people typically had large families. Often women had several children close together, then went a decade or more without modern contraception and without a pregnancy. When I inquired about birth control, some women replied “My husband takes care of me.” My wonderful nurse/translator told me that the couple was using withdrawal. Currently the Puerto Rican Total Fertility Rate is an incredibly low 1.1: most women on the crowded island are having only one child! Although withdrawal statistics show a high failure rate, this method seems to work well for some couples.
What makes it easier to halt female fertility rather than men’s? Remember from that 8th grade sex talk that women usually create one egg a month? Men make a thousand sperm every second! Egg production depends on a woman’s hormones working in an amazing, well-balanced sequence. It is fairly easy to disrupt the sequence with tiny amounts of exogenous hormones, as with the birth control pill.
In 1963 I met an assistant of Dr. John Rock, one of the developers of “the pill”. She told me that another of Rock’s projects was nicknamed “the Rock Strap”. Insulated briefs for men raised testicular temperature high enough to stop sperm production. Research along these lines is still ongoing in France.
The good news is that there are 4 new contraceptive methods for women. One is a hormonal IUD that is a little smaller and has less levonorgestrel than others, but is still effective for 5 years. It has a very low failure rate similar to other LARCs (Long Acting Reversible Contraceptives)–less than 1% per year. Kyleena® is similar to Mirena®, the first hormonal IUD, but may be better tolerated by some women because of its smaller size.
Currently, nonoxynol-9 is the most common agent used in vaginal spermicides. While the vagina is acidic and hostile to sperm, alkaline cervical mucus helps guide them as they swim toward fertilization. Phexxi, a new spermicide, is a “Vaginal pH Regulator” that is 90+% effective in preventing pregnancy. It also acts as a lubricant and may increase sexual satisfaction, but is expensive if you don’t have insurance.
Contraceptive diaphragms have been around longer than a century. They have none of the side effects of hormonal contraception, but their failure rate is higher. Although most diaphragms require fitting, Caya® is available in just one size and fits most women. It should be used with a spermicidal jelly or cream, like any other diaphragm. People with latex allergy can use it since it is made from silicone rubber. A Caya® costs about $85 and should last for years.
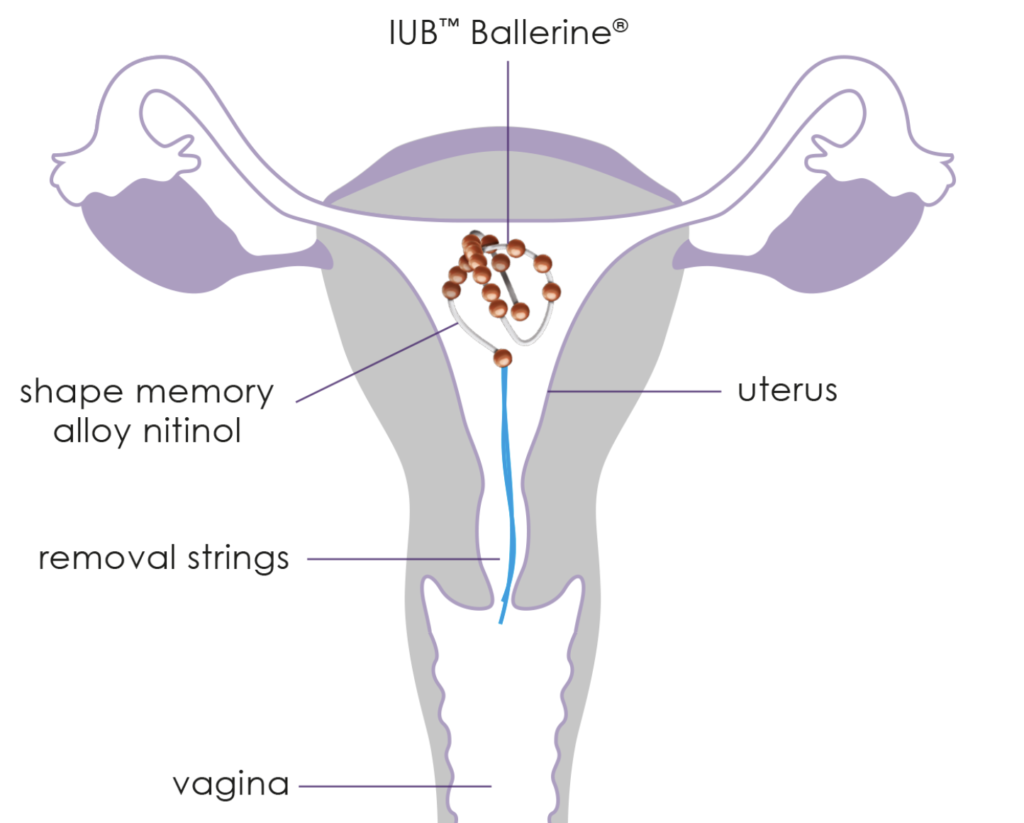
All IUDs currently available in the USA are “T” shaped. Most women tolerate them well, but some don’t. A novel IUD, Ballerine®, provides an alternative. Unique in design, a soft, springy strand in spherical shape has 17 tiny copper balls strung on it. The Ballerine® is straight in its inserter, then curls up to conform to the uterine cavity. It has been well received for a number of years in Europe and other countries where it has been used by over 94,000 women. Like other LARCs, fewer than one woman in 100 will conceive with Ballerine®, and its complication rate is low. Although not available yet in the USA, its manufacturer is planning to start the approval process soon.
Annovera® is a hormonal contraceptive vaginal ring that lasts a whole year. After it has been in place for 21 days, the user removes it for a week to bring on her period. It has two drawbacks: the cost, for someone who doesn’t have insurance, is about $2000! Also, the failure rate is higher than a LARC, although better than “the pill”.
With new contraceptive methods there is more choice–for women, at least. Please observe World Contraception Day, September 26th, whose purpose “…is to improve awareness of contraception and to enable young people to make informed choices on their sexual and reproductive health.”
© Richard Grossman MD, 2020